Tuesday, January 25, 2011
Poppy's gastrointestinal scare
Friday, December 17, 2010
Santa Paws for WHS
Thursday, October 28, 2010
A cautionary tale of chocolate toxicity for Halloween
Thursday, July 8, 2010
Caution for heat stroke
Summer Heat Dangerous For Dogs
Since we’re stuck in the middle of yet another heat wave in the mid-Atlantic region, I wanted to take a moment to warn dog owners about their pets’ risk of heat stroke. In the past few weeks a number of dogs have been brought into Friendship after collapsing due to heat stroke. Several dogs have even died, which is truly tragic since this could have been easily avoided.
One of the recent fatalities was a bulldog that was taken out for fifteen minutes around noon as part of a mid-day walk. He collapsed on his walk and was immediately rushed to Friendship. Sadly, despite aggressive treatment, complications from heat stroke damaged his organs so severely that he had to be euthanized the next day.

drawing by Robert Cole
What makes heat stroke potentially fatal is that the patient can develop a condition called disseminated intravascular coagulation (DIC) that causes massive and widespread damage to the blood vessels. This quickly results in multiple organ failure and the patient loses the ability to clot his blood. Treatment consists of aggressive supportive care and plasma transfusions, both of which are very expensive and not guaranteed to prevent death.
- Avoid taking your dog out during the hottest times of the day. (Quick rule of thumb: If it is too hot for you, then it is definitely too hot for your dog!)
- Keep an eye out for unusual behavior: If you are out in the hot weather with your dog and he slows down, lies down or acts reluctant to keep walking, you should let him rest, offer him cool water and head inside immediately.
- Make sure your dog has cool, fresh water available at all times.
- Never leave a dog (or any other pet) in a parked car when it is even slightly warm out. The temperature in the car can rise amazingly quickly and before you know it you have an overheated animal.
- Don’t take your dog running. (I am never a fan of running with your dog—check out this article to see why--but in this weather it is an especially bad idea).
Thursday, November 19, 2009
Urinary obstruction in cats

 On presentation Linus was moderately dehydrated, slightly depressed and his heart rate was lower than I would have liked at 180 beats per minute. During abdominal palpation I was able to feel a very large, hard bladder and determined that he had a urinary obstruction. After quickly placing an intravenous catheter we collected blood to check his electrolyte status.
On presentation Linus was moderately dehydrated, slightly depressed and his heart rate was lower than I would have liked at 180 beats per minute. During abdominal palpation I was able to feel a very large, hard bladder and determined that he had a urinary obstruction. After quickly placing an intravenous catheter we collected blood to check his electrolyte status.The potassium in his blood was dangerously high, which can lead to cardiac arrhythmias and rapidly result in death. We started Linus on IV fluids and gave him a medication to help lower his potassium. Because he was unable to urinate, the waste products normally excreted in urine were building up and making him feel sick.
I performed a cystocentesis which involves sticking a needle into his bladder to remove the urin
 e and relieve some of his discomfort. Because urinary obstruction is very painful for kitties, Linus was also given pain medication. X-rays showed he had stones in his bladder causing the obstruction. In male cats (and also male dogs), the urethra is very narrow, so it’s easy for things to get stuck in it. Stones are not the only cause of urinary obstructions in cats; mucus plugs, inflammatory cells, and crystals can also a blockage.
e and relieve some of his discomfort. Because urinary obstruction is very painful for kitties, Linus was also given pain medication. X-rays showed he had stones in his bladder causing the obstruction. In male cats (and also male dogs), the urethra is very narrow, so it’s easy for things to get stuck in it. Stones are not the only cause of urinary obstructions in cats; mucus plugs, inflammatory cells, and crystals can also a blockage.I used an injectable anesthetic agent to sedate Linus so a urinary catheter could be passed. This was necessary for many reasons. First, he needed to be able to empty his bladder. We also needed to start him on intravenous fluids to flush out his system. This would decrease the dangerously high levels of potassium and waste products he had been unable to eliminate. And finally, given Linus’s current state, he was at an increased risk for general anesthesia, so I wanted to stabilize him before going to surgery.
The next morning, Linus went to surgery to have the stones removed via a cystotomy. He was sent home the next day. Analysis revealed that his stones were struvite. This was great news, because this type of urolith responds very well to diet change and has a low level of recurrence. Linus started his new prescription diet and his owners report he is like a new cat at home.
Urinary obstruction is incredibly common and can quickly become fatal, so it’s important for all owners of male cats to be aware of the condition and its symptoms. If you ever notice your cat making multiple trips to the litter box, straining to urinate and vocalizing, please bring him in immediately.

Tuesday, November 17, 2009
Toby's Bladder Stones
Toby is a five-year-old Yorkie whose owner noticed he had blood tinged urine after he had an "accident" in the house. Toby's owner immediately brought him into Friendship on emergency. besides being worried about the bloody urine, she was also alarmed that Toby had peed in the house, since he had never done this before. I assured her he most likely had a urinary tract infection, and submitted urine for analysis and culture. I then sent him home with a broad-spectrum antibiotic. Though the urinalysis results would be available the same day, we would need to wait three to five days for the culture to come back.
I had the urinalysis results back an hour later. There weer some inflammatory cells, which you can see with an infection, but no bacteria present. I advised Toby's owner to monitor his closely; if the signs continued and the culture was negative, Toby might have bladder stones, also known as uroliths. It was very important that she make sure he was able to pass urine. Since male dogs and cats have a narrow urethra compared with females, stones have a tendency to get stuck in this area. This creates a urinary blockage and requires emergent treatment.
Thursday, October 29, 2009
A cautionary tale of chocolate toxicity for Halloween
 With Halloween this weekend and the holiday season just around the corner everyone will have more candy around the house than usual which is an invitation for curious pups to steal a snack. Dr. Dana Begnoche’s dogs Lola and Widget have volunteered to be used as an example for what can happen if your dog eats too many chocolates.
With Halloween this weekend and the holiday season just around the corner everyone will have more candy around the house than usual which is an invitation for curious pups to steal a snack. Dr. Dana Begnoche’s dogs Lola and Widget have volunteered to be used as an example for what can happen if your dog eats too many chocolates.Lola and Widget came in after breaking into the Halloween candy stash one afternoon. Milk chocolate, which consists mostly of cream and sugar, is generally not a huge concern unless massive amounts are consumed but dark chocolate is another story. Among other treats there was a bag of dark chocolate M&M’s missing and we were not sure how much each dog consumed.
An injectable medication was used to induce vomiting in both dogs so we could empty their system of as much chocolate as possible. Lola was the prime suspect as her heart rate was in the 200 beats per minute range which is too fast and she was very agitated. Chocolate contains theobromine and caffeine, which are both classified as methylxanthines. Unfortunately, dogs are sensitive to the effects of methylxanthines which can cause hyperactivity, increased heart rate, gastrointestinal upset, tremors, seizures and potentially death when ingested at a toxic dose.

Widget vomited a moderate amount of chocolate but was not showing any clinical signs of chocolate toxicity. He was given activated charcoal by mouth, fluids under the skin and an injection of Pepcid to help settle his stomach. The fluids would help flush out his bladder which is important since the methylxanthines are excreted through the urine and can actually be reabsorbed if allowed to collect in the bladder. Widget was sent home with instructions to take out frequently to urinate and monitor for any vomiting or diarrhea.
Lola vomited slightly more chocolate than Widget but she was showing clinical signs of chocolate toxicity which required more aggressive treatment. We started her on IV fluids and gave her a medication to help slow down her heart rate. Overnight we checked her heart rate every hour in case it crept back up again and she needed an additional dose. Lola was also given oral activated charcoal to bind any of the chocolate that wasn’t expelled when she vomited. Other than being anxious and whining all night Lola did great and was sent home the next morning.

There are a few take home messages in this tale. First keep the candy far away from nosey dogs, even if you don’t think they are interested in eating it. Second, know what kind of chocolate your dog has been exposed to. The higher the cocoa content or more bittersweet, the smaller amount it takes to reach a toxic dose. Finally if your dog does eat chocolate bring them in to see us immediately so we can induce vomiting to remove as much as possible from their system. Most of the time they do not need to stay in the hospital and can go home with you immediately.
Happy Halloween from Friendship! We hope you won’t have a chocolate toxicity story of your own this holiday season but if you do we will be here to help your dog vomit.
As a side note Lilly will be dressed as a bumble bee and Sparkle as a pig on Saturday. Poppy is refusing to keep on the costume I got for her, so instead she will be going as a very bad dog.
Tuesday, September 15, 2009
Hemoabdomen
When Brady arrived at the hospital he was able to walk but was very weak. His gums were an extremely pale pink--almost white--and his abdomen was distended – the classic signs of a belly full of blood, also called a hemoabdomen.
My suspicion was confirmed when I inserted a needle into his belly and pulled back a syringe full of blood. Because Brady was losing so much blood into his abdomen, he needed help to support his cardiovascular system, so we immediately placed an intravenous catheter and started him on fluids. His red blood cell count was predictably low as was his blood pressure; we needed to start supportive care to help him oxygenate his organs. He was given oxygen and a medication called hetastarch to help bring up his blood pressure.
After I was comfortable that Brady was receiving the supportive care he needed, I headed into a room to have what is always a very difficult discussion with his owners.
The most common cause of a hemoabdomen is a bleeding tumor in the spleen. Though there is a small chance that the tumor is benign, it is much more likely that it is a very aggressive type of cancer called hemangiosarcoma, a cancer of the cells that line blood vessels.
Not only was it most likely that this was a malignant tumor, there was also a strong possibility that it had already spread to his liver or lungs. Even though x-rays of Brady’s lungs did not show any metastasis, there could be microscopic disease present that just hadn’t become visible on x-rays.
His owners had three options at this point:
1) They could choose to euthanize immediately, reasoning that the tumor was most likely malignant and that it had spread, so that even if we went to surgery and removed it, Brady would need chemotherapy to treat the suspected metastasis.
My heart always goes out to the owners when it is necessary to have this overwhelming discussion. There are multiple options with varied outcomes and they need to make a life or death decision for their dog with very little time to think. After much discussion, Brady’s owners elected for him to have the emergency surgery.
In surgery, Brady’s abdomen was filled with blood from a large bleeding mass in his spleen. Fortunately, his liver was normal in appearance, so we proceeded to remove the spleen as quickly as possible to prevent further blood loss. I also took a sample of liver tissue to submit along with the spleen for review by a pathologist. Despite his severe anemia, Brady did very well during surgery and his recovery from anesthesia was uneventful.
Now we had to wait for the pathologist to send back the results of the biopsy samples. Six days later Brady’s owners were given a very happy and unexpected surprise: The mass was the benign form of disease called a hemangioma, and the surgical excision was expected to be curative.
I was thrilled for Brady and his owners, especially because after treating my own dog for hemangiosarcoma, I would not wish it on anyone. Unfortunately, this is not the usual outcome when a dog presents with a hemoabdomen and it is always a gamble no matter what decision the owner makes.
Thursday, August 6, 2009
Channey's angry pancreas
On physical exam Channey was very quiet, dehydrated, had a mild fever and was painful on palpation of her abdomen. My immediate thought was that Channy’s condition was caused by pancreatitis, a fairly common diagnosis or suspected cause of vomiting and diarrhea that many people do not know much about.
Pancreatitis is an inflammation of the pancreas, a gland that lives in close contact with the stomach, liver and small and large intestines. Its major function is to secrete enzymes that help digest nutrients in the small intestine.
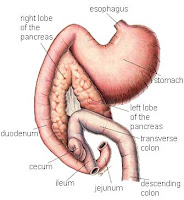
\Pancreatitis occurs when a breakdown causes the digestive enzymes to come into contact with the pancreatic tissue. This results in a large amount of inflammation that extends to the surrounding organs and, in severe cases, through the entire body. The most severe cases of acute pancreatitis can result in death, although this is uncommon.
 We are not sure what causes pancreatitis, but there are many suspected causes, with pet obesity and ingesting a very fatty meal being at the top of the list.
We are not sure what causes pancreatitis, but there are many suspected causes, with pet obesity and ingesting a very fatty meal being at the top of the list.My first step was to order x-rays, to find out if we could see what was causing the abdominal pain. Despite Channey’s recent steak-bone snack, I wasn’t expecting to see any bone fragments remaining, as these are usually digested very quickly. Still, I wanted to rule out any other abnormalities and make sure Channey’s small intestines had not formed a pattern consistent with obstruction. The x-rays were unremarkable which made me even more suspicious of pancreatitis.
Next, I submitted bloodwork and admitted Channey for supportive care. While I waited for Friendship’s lab to run her bloodwork, I checked a cPL snap test that specifically checks for one of the enzymes produced by the pancreas. Channey’s test was positive, confirming my diagnosis of pancreatitis. (Interestingly, this test is often negative, even in cases when I believe the dog still has pancreatitis. Yet another example of how important it is to look at how the patient is doing rather than rely solely on testing.)
I checked Channey’s bloodwork to assess the severity of her condition. She had a high white cell count consistent with inflammation and a high red cell count along with mild electrolyte abnormalities indicating she was most likely dehydrated. Fortunately, she did not have any elevations in her liver values, which can be another common finding with pancreatitis.

There is no specific treatment for pancreatitis - instead we try to alleviate the symptoms and make the patient more comfortable. We started Channey on intravenous fluid therapy to re-hydrate her and antibiotics to help with the diarrhea. Pancreatitis itself is not infectious but severe diarrhea can lead to secondary bacterial infections. To help keep her comfortable, we gave her pain medication along with anti-nausea medications. She was not offered food for twenty-four hours to allow her gastrointestinal tract time to rest and the inflammation to decrease.
Channey was in the hospital for about two and a half days before she began to improve. She started eating the small amounts of bland diet we offered her and was able to keep it down. By the fourth day we had transitioned her to oral medications, she was eating well without vomiting and appeared one hundred percent more comfortable. She went home with suggestions for weight loss and strict instructions to avoid any fatty foods.
Tuesday, January 6, 2009
Welcome to Friendship Tails!

Before attending vet school I graduated from Vanderbilt University with a degree in mechanical engineering. It wasn’t until I was out of college for a few years that I realized becoming a veterinarian was the perfect career path for me. I spent the majority of my childhood and high school riding horses and at home I was always surrounded by our many dogs. I never truly understood the remarkable bond that one can have with a pet until I met my dog Westin, golden retriever mix. She has been my best friend since college after I found her as a puppy living on the streets in the Bahamas. My relationship with Westin has inspired me to become a veterinarian so that I can help others experience the unconditional love and fulfillment that a pet can bring to your life.
I live in Northwest DC with my three dogs, Westin, Sparkle and Lilly and three cats, Vegas, Breaker and Furla. The kitties are rescues I met while working at the animal shelter in vet school. Sparkle is a rat terrier and is very talkative and feisty; she apparently has an opinion about everything. Lilly is a Chihuahua mix I found playing in train tracks on the side of a highway in Florida and is by far one of the cutest dogs I have ever met (I could be biased). Needless to say with this crew there is never a dull moment in my house.
My goal in creating Friendship Tails is not only to inform the community about all the amazing things that happen at Friendship but to offer a source of reliable information for pet owners. Every doctor at Friendship is committed to providing the highest quality of medicine for their patients, the technicians work tirelessly to make sure everyone is given the best care possible and the front desk staff ensures everything runs smoothly. In addition to what we do at the hospital Friendship is also very active in the community with close ties to Washington Humane Society, Washington Animal Rescue League and DC Animal Control.
Apart from what an exciting place Friendship is I also want to educate pet owners so that they can work with their veterinarian to ensure a long and healthy life for their own dogs and cats. I find that my clients often have the same questions and concerns regarding their pets medical needs, I hope Friendship Tails can answer some of these questions. I would be lost without the animals in my life; let me help you care for the pets in yours.
--Ashley Hughes, DVM