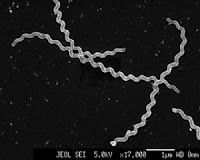
After a long night during which no one in the house slept very well, Huey’s owners brought him to Friendship. He was quickly diagnosed with kennel cough, which is a collective term for a highly contagious group of viruses and bacteria that cause irritation in the upper respiratory tract. Symptoms include coughing, sneezing, watery eyes, nasal discharge, lethargy, decreased appetite and fever.
Although Huey had a nasty cough with frequent sneezing, he did not have a fever and was otherwise eating and acting like himself. I prescribed a cough suppressant and advised his owners to give him steam baths at home to help soothe his airways. The cough suppressant would allow Huey to rest, thus preventing his immune system from becoming stressed, which in turn could lead to a secondary bacterial infection.
The infection would most likely resolve without treatment, although Huey's cough might last for 7-10 days. I instructed his owners to watch him closely for lethargy, decreased appetite, a yellow/green discharge from the nose, or a fever greater than 103 degrees. These are signs of a secondary bacterial infection which would need to be treated with antibiotics.
Huey’s owners asked me about starting antibiotics immediately, but I explained that Bordetella (the bacteria most commonly associated with kennel cough) is not very responsive to antibiotics. In addition, most of the other infectious agents that cause kennel cough are viral, and therefore cannot be treated with antibiotics.
Since Huey had previously been vaccinated for kennel cough, his owners wondered how he could have contracted it. I told them that the kennel cough vaccine does not actually prevent the disease. Instead, it helps boost the immune system to decrease clinical signs and probably prevented Huey from getting even sicker.
The worst part for Huey was that since kennel cough is highly contagious, he wouldn’t be able go to the dog park or doggie day care until 7-10 days after his cough had fully resolved. His owners called a few days later to report he was doing great and they were happy we held off on the antibiotics.












 I strongly recommend the Lepto vaccine for all my canine patients, and my own dogs are vaccinated, too. I frequently take my dogs to the park and trails in my neighborhood, and feel much more comfortable knowing that I’ve done everything I can to protect them
I strongly recommend the Lepto vaccine for all my canine patients, and my own dogs are vaccinated, too. I frequently take my dogs to the park and trails in my neighborhood, and feel much more comfortable knowing that I’ve done everything I can to protect them

 Before the procedure we perform a complete physical exam. We listen to the heart to make sure there is not a heart murmur or abnormal rhythm, and we listen to the lungs to make sure they are are clear. We also make sure that pre-anesthetic bloodwork has been done in the past three months. Bloodwork allows us to evaluate the liver and kidney values of the patient. It is important that these two organs are functioning well, because they are responsible for processing the anesthetic drugs. A complete blood cell count (CBC) is included to check for low platelets that could result in excessive bleeding; decreased red cells indicating anemia; and an increase white cell count which could indicate infection is present.
Before the procedure we perform a complete physical exam. We listen to the heart to make sure there is not a heart murmur or abnormal rhythm, and we listen to the lungs to make sure they are are clear. We also make sure that pre-anesthetic bloodwork has been done in the past three months. Bloodwork allows us to evaluate the liver and kidney values of the patient. It is important that these two organs are functioning well, because they are responsible for processing the anesthetic drugs. A complete blood cell count (CBC) is included to check for low platelets that could result in excessive bleeding; decreased red cells indicating anemia; and an increase white cell count which could indicate infection is present.

 Once the patient is fully sedated, we use the intravenous catheter we placed at the beginning of the procedure to administer powerful anesthetics called "induction drugs." These drugs completely relax the patient's throat, so that we are able to painlessly insert an endotracheal tube -- known for short as an ET tube (pictured above). We use the ET tube to administer gas anesthesia, and also to help keep the patient breathing freely.
Once the patient is fully sedated, we use the intravenous catheter we placed at the beginning of the procedure to administer powerful anesthetics called "induction drugs." These drugs completely relax the patient's throat, so that we are able to painlessly insert an endotracheal tube -- known for short as an ET tube (pictured above). We use the ET tube to administer gas anesthesia, and also to help keep the patient breathing freely.