A few weeks ago, I noticed that one of my cats had begun vomiting at least one a day. After a couple of days of observation--and one morning of being woken up to the sound of vomiting--I determined that it was my cat Breaker.
All cat people know that cats vomit from time to time, and there are about a million things that can cause it. But when a kitty starts vomiting more than once a week, it warrants further investigation. I started by giving Pepcid AC to Breaker once a day, to help settle his stomach by decreasing the amount of stomach acid produced. Unfortunately, despite the Pepcid, I continued to find frequent piles of kitty puke around the house.
It was time for some veterinary detective work: My first step was to run bloodwork to check for the most common cat ailments:
kidney disease,
hyperthyroidism and liver disease. I also submitted a feline heartworm test. The good news was that the bloodwork was unremarkable and Breaker tested negative for
heartworm disease.
My next step was schedule an abdominal ultrasound to look for signs of pancreatitis, inflammatory bowel disease (IBD), and lymphoma. Luckily for Breaker, Friendship’s internist
Dr. McConnell happens to be an absolute genius with this diagnostic test.
The ultrasound is non-invasive and, other than a little abdominal pressure, not painful. It allows us to view the internal architecture of the abdominal organs. Where x-rays show shapes and shadows, ultrasound lets us assess such things as the layers in the intestinal wall, and see if the gall bladder is distended or the bladder wall is thicker than it should be.
I was relieved to see that Breaker’s pancreas did not appear inflamed, his abdominal lymph nodes were normal sized and his intestinal wall looked just like it should. Because ultrasound is not one hundred percent diagnostic, I still didn’t have an exact answer as to why my poor kitty was vomiting. Still, it was good to know that pancreatitis, IBD, and lymphoma were much less likely.
To further rule out pancreatitis, we submitted a blood test to the vet school at Texas A&M to check Breaker’s pancreatic values. These turned out to be normal. At the same time, we decided to see if a change in diet would help. Success! I’m pleased to report that I switched Breaker to a prescription diet, and he hasn’t vomited once.
My plan now is to monitor him at home and continue with the new diet. If he starts vomiting again the next step would be endoscopy, which is the least invasive way to collect biopsy samples of the stomach and small intestine. This would then allow us to distinguish between inflammatory bowl disease and lymphoma. Let us hope for no more kitty vomit from Breaker.

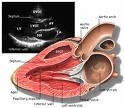 It could mean nothing or it could indicate that there is heart disease present. The only way to know is with an ultrasound of the heart called an echocardiogram. This procedure takes around 30 minutes and is done by a board certified cardiologist. Usually sedation is not necessary and you are with your pet the entire time. The doctor will image the heart and see if there is disease present such as thickening of the heart wall or abnormalities with the valves.
It could mean nothing or it could indicate that there is heart disease present. The only way to know is with an ultrasound of the heart called an echocardiogram. This procedure takes around 30 minutes and is done by a board certified cardiologist. Usually sedation is not necessary and you are with your pet the entire time. The doctor will image the heart and see if there is disease present such as thickening of the heart wall or abnormalities with the valves.